Intern Encyclopedia
Setting Up A Surgery ("PCS")
Preop
TIP: Put all these orders in a dedicated PRE-OP folder in your favorites and it will take you < 10 seconds. Order everything STAT and give nurse a courtesy call kindly saying this needs to be done tonight and not with AM labs. Consolidate all orders so patient is stuck only once.
Very little known fact: nurses cannot actually draw blood from standard peripheral IVs (the veins blow out), those are generally reserved for injecting drugs!
- Within hospitalization: CXR, UA, EKG
- Within 72 hours of surgery: T&S, CBC/BMP, Coags (PT/PTT/INR)
- Midnight before: NPO, DVT ppx off, IVF on (use MD Calc maintenance fluid calculator for the rate)
- Pre-operative risk stratification if patient is not an elective case that is coming from SDS
- CPC is always preferred but only works business hours (no weekends/evenings). Tiffany from CPC is the PA and is great, give her a courtesy call and if you have multiple patients give her a prioritized list.
- Med A is the backup if needed overnight/weekends. You must consult AND page them if it is needed overnight. Don't be a gome and say "can you clear for surgery" without knowing anything about the patient. Have a quick high level understanding of their systemic health (cardiac/respiratory and liver/kidney function) status and social history (smoker/drinker) and ask them pre-op risk stratify. THIS CONSULT ALSO MUST BE SIGNED OUT TO NIGHT FLOATER.
- (Nitin patients): Order the preop neurosurgery powerplan "Preop Neurosurgery Powerplan"
IMPORTANT: ORDER ALL THESE THINGS ASAP TO GET THE WHEELS ROLLING AND ENSURE ALL IS COMPLETE BEFORE YOU SIGN ANYTHING OUT TO NIGHT FLOATER. It is your responsibility not merely to order these things, but to ensure they are completed and resulted in the chart and if absolutely necessary sign out to the night floater (although you really want to avoid that). Moreover it's also your responsibility to follow-up on the actual results and act as appropriate, e.g. if the pt has a UTI then it needs treating, an arrythmia then senior needs to know and pt will need a cardiology consult
If you are signing anything out to night floater, you need to call nurse and kindly ask that they get things done, that is not something you can dump on night floater.
Consent
- Must include patient stickers on at least every first page of every consent form or otherwise write name/MRN.
- For every surgery: print out (1) general consent form (2) surgery-specific consent form (if it exists) (3) blood consent form
- every spine procedure: include the phrasing "with additional levels as needed"
- every procedure with sidedness use the phrase "left possible right" unless it is very obvious you will do one side (e.g. crani)
- ⚠️**EXCEPTION TO ABOVE: For Moossy, list only specific procedure on consents. No possibles.
No abbreviations anywhere (especially Blue consents)
INCLUDE SIDEDNESS where appropriate
- Take a picture of the consent form being placed into the correct patient chart (binder)
- If patient is in ED: not sufficient to put completed consent in the chart, they may lose it. You still put one there, but once a consent is completely filled out (signed and witnessed), make a copy in ED and put the copy on clipboard in resident lounge).
- Even if it was a moonlighter/trauma junior who should have consented the new consult, it's your responsibility to personally check if the patient is on your service. You can kindly ask them if the patient still needs consent or just go check the patient's binder yourself.
Schedule
- Call OR scheduler 412-647-3345 if non-emergent next-day surgery
- Call OR Front Desk 412-647-3270 if surgery is in next 24 hours or on weekend / evening
- If you want to book a case for weekday but it is the weekend, then call OR scheduler and leave a message with the following info:
- Attending
- Patient name and MRN and location
- Your name, role, and pager #
- Procedure
- All off the info below (image guidance / C/O arm, instrumentation, position, ETA)
- can also email PUHORScheduling@upmc.edu
- Always confirm they actually post it by checking assigngen.upmc.com
Have the following info ready before you call (ask your Chief/senior if unsure, do not guess)
- Image guidance needed? (if applicable)
- C-arm/O-arm needed? (if applicable, e.g. spine)
- Patient position: (prone vs. supine)
- How will head be stabilized? Horseshoe vs. Mayfield w/ pins
- Do you need a radiolucent Mayfield?
- Special operating table/frame? (e.g. Jackson Table with Wilson Frame)
- Neuro-monitoring (SSEP? Uppers/Lowers/etc)
- Spine Instrumentation company - this is crucial as it is attending specific and the reps from each company are NOT always at Presby unless told the day before)
- How much time it will take - in reality this doesn't matter as they will just use the average case length for that attending but you need to have a ballpark (e.g. 1 hr vs 10 hrs)
| Spine Attending | Instrumentation Vendor |
| Hamilton | |
| Buell | |
| Okonkwo | |
| Gerszten | |
| Agarwal | |
| Moossy |
Sign-off template
Example of a sloppy sign-off that generated a re-consult the next day.
Plan A - Cranial
Will vary per attending and service, but these are generally universal common orders.
Plan A - Spine
Will vary per attending and service, but these are generally universal common orders.
Workflow for discharging a patient
See Rehab slides in Orientation 2023-24 powerpoint.
Generally speaking, every patient needs clearance to safely go home from PT / OT after surgery. Exceptions are when patient is extremely well-appearing and attending simply doesn't care.
Steps to sending someone home
1. PT / OT Consult ("comprehensive rehab services)
- Should happen on POD1
- Order as "discharge today" to force PT and OT to see them, but don't abuse this.
| Verbage in PT / OT Form | Interpretation |
| N | Home |
| intermediate | SNF |
| comprehensive / intensive | IPR |
Jump to step 3 if SNF or Home.
2. PMR Consult
- generally speaking you only place PMR consult when PT / OT recommends it.
- However some people get an "early PMR consult" when they will clearly need rehab e.g. TBI who will definitely need BIM. Many DOO patients will fit this category.
- Trauma Rehab rounds are when we fight for borderline patients to go to rehab.
NOTES FOR ACCELERATING DISPO TO REHAB:
- Make sure trach is cuffless (see below for how to check)
- Turn off labs if not needed, you're looking for trouble.
- Take patients off IVF and IV pain meds ASAP.
- Document medically ready for discharge in your A & P.
- Generally speaking PMR will require PT / OT recs within 72 hrs of discharge.
- If someone has a white count and are taking steroids, just document it's likely from steroids
- Can always give fluid bolus to dilute a CBC if no clinical concern.
3. Case Management
IPR:
SNF:
Home with assistance (HHPT / HHOT):
- Order Home care ASAP
- Ask care manager to order durable medical equipment.
- See discharge instructions (TBA)
Home with outpatient PT / OT
- See discharge instructions (TBA)
Home without assistance:
- just send them home
High yield pharmacology guide
Can always call inpatient pharmacy for help - see contact number for every PUH floor in the phone book.
| Drug | Dose and Route | Use | Notes / Tips |
| Robaxin | |||
| Flexeril | |||
| Lyrica | |||
| Dilaudid PRN | |||
| Dilaudid PCA | pt dose 0.1 mg RN bolus (breakthrough dose) 0.2 mg 1 hour limit: 1 | Ordered as "PCA Dilaudid Powerplan" D/c loading dose that comes with powerplan Patient admin dose = | |
| Oxycodone IR | 2.5 mg 5.0 mg prn moderate 4-6 pain 10 mg prn severe 7-10 pain | For discharge Rx: generally, ordering 5mg tabs x 28 will be the most painless for you, as more will require insurance authorization. | |
| Dexamethasone | MUST ALWAYS RX PEPCID AND SLIDING SCALE INSULIN! | ||
| Reglan | |||
| Antiemetic that starts with a G | use for intractable even with Zofran | ||
| SQL | |||
| SQH | |||
| Labetalol | PRN for CAP | ||
| Hydralazine | PRN for CAP | ||
| Topical Lidocaine | |||
| Zofran | |||
| Topical lidocaine with epi | |||
| UTI for males | |||
| UTI for females | |||
| K+ | PO: IV: | ||
| Ca2+ | IV | ||
| Mg2+ | PO: IV: | ||
| PO43- | PO: IV: | ||
| Gatorade | mild asymptomatic hyponatremia | ||
How to answer "Are you guys okay for toradol / NSAIDs"
TBA
How to drug people for an LP
Try not to, but if you must you can use one of these on the floor without ICU team.
| DRUG | DOSE AND ROUTE | USE FOR |
| Lido with epi | Needle-site pain, especially if anticipate you will try multiple levels as the bottle in LP kits has a very small volume adequate for only one level. Order this and ask nurse to get it ready on every single patient but don't open unless needed | |
| Fentanyl | 25 mg IV for normal sized adult can go up to 50 mg IV for large people (>100kg) If no access, same doses intranasally will work | |
| Ativan (Lorazepam) | 0.5mg-1mg PO or 0.5mg-1.0mg IV | |
| Ketamine | 0.3 mg/kg max of 35 mg over 15 minutes in an NS bag | only use if in the ICU; key is to push it slow to not cause laryngospasm! This rate is slow and likely will be ok on the floor. |
How to drug people for an MRI
MRI will frequently page you that a patient is freaking out/ in too much pain to sit still for an MRI.
Return the call immediately and dose one of the following drugs.
Remember rules for conscious sedation at PUH only allow you to dose 1 at a time w/o ICU presence and certainly with just an MRI nurse (see below).
TIP: if you know a pt is likely to freak out or be in too much pain to stay still, order one of the drugs below PRN and specify in comments to use in MRI if needed (save yourself a page).
NOTE: when ordering any of these drugs which may depress respiration, there is no harm in playing it safe and just putting the patient on a cardiac monitor with pulse ox. This is something that can easily go into the scanner with the patient, no reason not to do it.
| DRUG | DOSE AND ROUTE | USE FOR |
| Valium | 5mg PO, 2.5mg IV | Anxiety / Agitation / claustrophobia |
| Dilaudid | 0.2mg IV (0.5 if large / non-opioid ideally, naive only if "<65") | Pain |
| Ativan | 0.5mg-1mg PO or 0.5mg-1.0mg IV | Anxiety / Agitation / claustrophobia |
| Zyprexa (olanzapine) | start w/ 2.5 P.O. if geriatric / small / TBI up 5.0mg ODT/IM if excessive agitation / large up to 10mg max | Agitation |
How to intubate people for an MRI
- Coordinate this with charge anesthesiologisy 412-647-4441 and Presby MRI (# in phone book)
Steps BEFORE Every Case
- Kindly ask circulating nurse to man your pager, put your phone down on their COW and give them your phone code if you are using SPOK mobile.
- Tell them to please call back every page and "make sure it is not urgent." It is always YOUR judgement of what is urgent (not theirs) so ask them to inform you of every single page as it comes in. If you have to scrub out you have to scrub out.
Steps AFTER Every Case
- Log your case
- Ask attending/senior resident (ask during case/right at the end):
- Ok for foley out?
- Any specific orders you want besides routine Ancef/pain/bowel/antiemetics?
- Any CAP?
- ICU vs floor (if it's not obvious)
- Will this patient need a feeding tube we can just place now?
- Write an immediate post-op surgical note documenting:
- Procedure and pertinent complications (e.g. CSF leak repaired primarily vs. duragen or EBL > 3L)
- Drains - must label each with a letter and document side each drain is on as well as location in the closure. For example
- Drain A - LEFT - subfascial
- Drain B - RIGHT - supra-fascial
- THIS IS CRITICAL ESPECIALLY IF THERE IS A CSF LEAK
- Cultures:
- Path/biopsy/results:
- Closure:
- Flaps/Packings:
- Med rec if patient is coming from SDS (do not dump this onto the service residents). Restart or hold all home meds.
MEDICATION RECONCILIATION
- First of all, you can only do this after the nurse has done a medication history upload - this is not your job, call the nurse/charge and ask them to promptly do it so you can medrec them
- It is especially important to ask about use of anticoagulants (aspirin, Coumadin, Plavix, Eliquis, Xarelto, Pradaxa), steroids, and antiepileptics
- Ask attending or chief for plan for each of those meds. The importance of this step cannot be understated!
- The attending will almost always hold anticoagulation at admission, unless the patient has an intracranial stent, aneurysm coil, or symptomatic carotid stenosis
- If the patient doesn't know what meds they're taking and at what doses, call the patient’s pharmacy (ask nurse/charge to do that)
STANDARD POST-OP ORDERS ON EVERY SINGLE CASE YOU DO
SPECIFIC POST-OP ORDERS (IF APPLICABLE)
NOTE: you may need to give a loading dose of a med followed by scheduled dosing. Be sure to start the scheduled dosing one time interval after the loading dose
- E.g. 1 dose dexamethasone 10 mg ONCE STAT followed by 4q6 starting 6 hours after the loading dose
- E.g. 2 Phenytoin: 20/kg loading dose, then 100 q8 starting 8hours after the loading dose
SIGNOUT TEXT MESSAGE
- Before leaving OR and even before pt wakes up for an exam, text-sign out to all resident and APP members of service the patient is on (chief, senior, and junior) using following template (remove bullets if not applicable)
POST-OP TEXT SIGNOUT TEMPLATE- Patient Name
- Attending initials
- Procedure and pertinent findings/complications (CSF leak/ high EBL?)
- Drains, specify suction type and location in the closure (e.g. LEFT subfascial)
- CAP < _____ (or lack thereof)
- MAP
- Cx (specify pre or post- ABx or wash)
- Pertinent lines (e.g. foley until 6AM POD1)
- Post-op Imaging
- Any abnormal activity restrictions/Bracing rules (e.g. TLSO precautions)
- Immediate labs to follow-up on (e.g. DIC labs)
- Admit to floor vs. ICU
- Exam to follow (then text exam as soon as patient wakes up, noting any pertinent pre-op deficits as applicable)
TIP: this is a long text so for your efficiency, you can email this to yourself on the computer and send it from your phone as a text.
- Call or text attending to tell them how patient woke up. Better yet if they are in another OR, find out and let them know personally if at an appropriate part of case. Do not call much less text Moossy, find him around PACU or surgeon's lounge.
- Transport patient to ICU directly vs. drop off at PACU (if patient is going to floor)
Transporting and signing out a post-op patient
OPTION 1: If patient is going straight to the floor post-op, you deliver them to the PACU and they take it from there.
- How to sign-out to PACU nurse / ICU nurse
- What procedure you did and why
- Number and location of incisions and what they are dressed with
- Drains, specify suction vs. gravity
- Pre-operative deficits if applicable
- CAP / MAP floor if applicable (or lack thereof)
- what imaging is ordered and whether the patient needs imaging done by PACU nurse before leaving PACU to floor
OPTION 2: If patient is going straight to the ICU post-op, you deliver them straight to the ICU. If you must get a scan on the way to ICU, you must accompany everyone to scan and then drop off to ICU. This is why you ask attending if they truly are concerned enough to get a scan literally on the way to ICU (meaning anesthesia from OR must go with you) versus dropping off at ICU and having ICU nurses/CCM take the patient (often the latter is enough).
- How to sign out to ICU CCM and ICU Nurses: need to make sure both nurses and CCM are present!
- Start by calling the ICU CCM as you roll out of the OR. Even if anesthesia gave nurse heads up, CCM is not always aware and would appreciate the call, plus you save yourself time by having them ready when you arrive. Never hurts to over-communicate.
- CCM 6FG: F-side (beds LOW 1-10) 578-9460, G-side (beds 11-20) 864-1521
- CCM 4F/5F: 692-2193
- CCM 4G: 864-2373
- What procedure you did and why
- Number and location of incisions and what they are dressed with
- Drains, specify suction vs. gravity
- Pre-operative deficits if applicable
- CAP / MAP floor if applicable (or lack thereof)
- what imaging is ordered and whether the patient needs imaging done by PACU nurse before leaving PACU to floor
- SPECIFIC ICU SIGN-OUT
- CRITERIA FOR EXTUBATION (e.g. "we'll call you if scan looks good")
- All pertinent orders (labs/imaging needed) and whether they are ordered or need ordering
- Start by calling the ICU CCM as you roll out of the OR. Even if anesthesia gave nurse heads up, CCM is not always aware and would appreciate the call, plus you save yourself time by having them ready when you arrive. Never hurts to over-communicate.
How to preround
| Type of post-op patient | Questions to ask patient while pre-rounding |
| ALL | 3Ps: Pee? Poop? Passing gas? Pain: You had pain in X location before surgery, how does it feel now, show me where it is? Home: Do you want to go home? |
| Spine | Pain |
| EEA | Any leaky clear fluid? |
Cranial patients pre-round
Orientation, Pupils, EOMs, visual acuity, visual fields (for sellar/suprasellar lesions), facial sensorium (get a percentage if decreased)
Facial muscle strength (central facial vs. cranial nerve)
(House Brackman Score of CN VII dysfunction, palatal elevation/intact gag and shoulder shrug for lesions involving the CPA angle or lower)
Hearing, Tongue Symmetry, Upper Extremity Drift (present or absent)
Following Commands?, ataxia/dysmetria (present or absent).
How to present
1) Attending
2) Numbers/1 liner (Op day 2 procedure day 1 bleed day 0 etc)
3) Drains
4) Vitals
5) Meds (state presence of SQH or other blood thinners first i.e “on SQH and aspirin”)
6) Labs/Culture/Micro results
7) Exam
8) Non-service consults like PT nutrition recommendations as applicable
9) Other consults recommendations as applicable
10) Plan for the day
Neuro exam template
Cranial Nerve Exam
Cranial Nerve 7 (QID 21511)

Motor Exam
| RIGHT | LEFT | |||||||||
| UPPER | D (C5) | B (C5/6) | WE (C6) | T (C7) | HI (C8) | D (C5) | B (C5/6) | WE (C6) | T (C7) | HI (C8) |
| 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | |
| LOWER | HF (L2) | KE (L3) | DF (L4) | EHL (L5) | PF (S1) | HF (L2) | KE (L3) | DF (L4) | EHL (L5) | PF (S1) |
| 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
Post-Angio Check
TBA
How to setup patient for angio
All angio procedures can be done on SQH/SQL unless otherwise stated
- Place DSA consent in chart
- NPO at midnight
- Check for contrast allergies (ask patient, search Epic)
- Order Neuro IR consult
- Send the following email to fellows
To: suryadevaran@upmc.edu, kayyalimn@upmc.edu, fadhila@upmc.edu
cc: neurosurgResidents@upmc.edu
Attending:
Patient:
Location:
DOB:
MRN:
Indication: Insert blurb
Consent in chart, NPO at midnight, no known contrast allergies, NIR order in
How to coordinate shunt with general surgery
- Place a general surgery consult ASAP and page general surgery to discuss (make sure you have h/o abdominopelvic surgery or lack thereof handy before you call them)
- Email Kenneth Lee MD (Gen Surg) the following email
You can also expand your initial email to include all the other general surgeons if Lee does not answer in time (or just email everyone off the bat)
Brown, Joshua <brownjb@upmc.edu>;
Forsythe, Raquel M <forsytherm@upmc.edu>;
Leeper, Christine <leepercm@upmc.edu>;
Neal, Matthew D <nealm2@upmc.edu>;
Sperry, Jason L <sperryjl@upmc.edu>;
Zuckerbraun, Brian <zuckerbraunbs@upmc.edu>;
Gregory Watson watsong@upmc.edu
Hello Dr. Lee,
Dr Neurosurgeon is requesting your assistance with a VPS for a patient on DATE AND TIME AND OR#.
Name:
MRN:
DOB:
Clinical history:
Insert Blurb from TRAC including Age, Dx, procedures, etc.
History of abdominopelvic surgery: this is the most important part of your email for them. Tell them if there is abdominal history or lackthereof (to your knowledge).
We would appreciate your counsel on whether this patient would be an appropriate candidate for a VP shunt and if you are available to assist on INSERT DATE TIME AND OR#.
Thank you,
How to schedule IR-guided LP or CT-Myelogram at PUH
- A PA named Megan doese these down in general IR
- Her number is 578-9430
- Call her to schedule
NOTE: •spine procedures such as lumbar drains, blood patches, injections, discograms, biopsies, etc - are performed by Dr. Agarwal not the myelo service, despite all of us working within Neuroradiology.
How to schedule inpatient EMG/NCS at PUH
- Find out exactly which extremities you want EMG/NCS of. They will never do all 4 extremities both because its impractical and unnecessarily painful. Generally they will do one upper and one lower, and you need to specify side if unilateral symptoms.
- Dr David Lacomis (lacomisd@upmc.edu) is generally the guy who will do these. (don't send wrong email to his son Christopher Lacomis)
- when he is not on, there is someone from PM&R and neurology who does them
- Erika Coury (courye@upmc.edu) is the lead EMG tech and will help you find another attending if Lacomis is not on
- Numbers to call are 412-647-7730 or 412-647-5424.
To: courye@upmc.edu, lacomisd@upmc.edu
cc: Chief, senior, NSG attending
Hello Dr Lacomis and Erika
PATIENT (MRN) is a BLURB
Diagnosis:
Most recent exam:
Dr ATTENDING is requesting that you perform EMG/NCS of WHICH EXTREMITIES. Can you please let us know if you can do this test inpatient as soon as possible?
Thank you in advance for your help.
How to stand a patient for an Xray
This is ok to do as long as there is no unstable spine on CT / MRI. As long as you can push the patient through the pain, load them up with some dilaudid right before. Often this will be the difference between operative / conservative management.
How to call a condition C (critical) at Presby (Orange bag)
IDEALLY: Ask nurse to print Rounding Report III / Code sheet (on Powerchart: highlight patient in the list, right click TASK in upper left --> Reports --> Choose Rounding Report III )
1. Be on the floor next to patient right away! You can ask charge / huq on the floor to call it for you.
Once the orange bag (either an APP or CCM Fellow) arrives, present in the following order
2. "I called the condition for ______ (e.g. I called for AMS)"
3. Relevant VS (O2 sat of 60%, etc.)
4. "I have done ____ for the patient" (or nothing - which is ok)
5. They were originally admitted ______ days ago for _______ (e.g. mGLF w/ SDH). Have TRAC info handy and be ready to answer all pertinent PMHx/PSHx.
6. Stick around for orange bag's questions. Give orange bag your number so they can easily reach you as needed. Once you have handed off to the orange bag, it is safe, legal, ethically acceptable for you to leave to do your other work. You do not need to stick around forever.
How to call a stroke condition at Presby
1. Call condition C (see above) so CCM (orange bag) is available to address ABC needs during scans
Before orange bag arrives, have all the info ready for orange bag:
2. Ask nurse to get POC glucose
3. Ask nurse to get monitor if not already on. If takes too long, have PCT come get vitals STAT before orange bag arrives.
4. Must know if on AC/AP
5. Should know last known well (NOT the time you found symptoms, but truly the last known well in the literal sense)
Once orange bag arrive
Same as above for condition C, but make sure know exact neuro deficits.
How to place a duo-tube
Orders:
- Dobb-Hoff Tube tube
Step 1: Ask Nurse to do it
Step 2: Ask Duo-tube team to do it
Step 3: Try it yourself
Step 4: Consult ENT
How to order tube feeds
Orders
1. "Dobb-Hoff Tube" is a Duotube
2. "XR Abdomen 1 View Exam" to ensure feeding tube placement is checked (confirm placement ok on XR either yourself or final read or with your senior before starting tube feeds - can do the orders below and then just put a nursing communication note saying don't start TFs until XR done and reviewed. They should know this too but don't assume).
3. Tube Feed Power-plan
- Keep all the auto-checked parts of the powerplan checked
- 3A) Choose a specific Tube Feed. If diabetic, choose Diabetisource. Otherwise if kidney function is fine, choose Impact Peptide 1.5 or Isosource.
Generally you can start tube feeds with the powerplan on your own at a low rate. Part of the powerplan is a nutrition consult, they will review your choice of tube feed and rate to make sure everything is ok and you can adjust accordingly.
Selecting a Tube Feed Food Formulation - EMCrit Project
| Tube feed choice | Reasons for use / comments |
| Diabetisource AC | Diabetic default |
| Impact peptide 1.5 | Make sure they have good kidney function if you have to choose this. Avoid in sepsis but good for post-trauma and post-op patients. |
| Isosource 1.5 | Good #1 choice |
| Jevity 1.2 | Good #1 choice |
| Nepro Carb steady | Good for significant AKI / CKD (lower protein and K+) |
| Osmolite | Good #1 choice |
| Nutren 2.0 | Anything that's 2.0 is good for the fluid-restricted. |
| Kate Farms | this is the equivalent to a GI easy if someone having diarrhea. |


- 3B) Choose a specific modular / additive. Safe to just choose 1 Prosource packet per day until Nutrition tells you otherwise. If Diabetic, choose Arginaid (powder)

- 3C) Tube feeding flush
- 30q4 is generally ok, just to maintain tube patency
- This is not the same as free water flushes (see below) which is actually used to regular sodium
- 3C) Free water flushes
- these are not checked by default in the powerplan, you must choose
- these actually matter and both the flush content (NS vs water) and frequency will change the patient's sodium
- Generally ok to start with
-
- d
How to handle Answering Service like a champ
Algorithm for every call
TBA
How to inject drugs intraventricularly (into EVD)
TBA
How to place a duo-tube
Orders: Duo-Nebhoff tube.
Step 1: Ask Nurse to do it
Step 2: Ask Duo-tube team to do it
Step 3: Try it yourself
Step 4: Consult ENT
How to remove cranial drains
Cranial drains will be JP drains or subdural bags.
| MATERIALS | PROCEDURE |
Materials:
| Do a mini time-out with yourself. Confirm the patient, room #, and location of drain you're removing! While Unsterile
Sterile
+/- post-pull CTH as warranted (per chief) - TELL NURSE AND PLACE ORDER |
How to remove EVDs
| MATERIALS | PROCEDURE |
Materials:
| Do a mini time-out with yourself. Confirm the patient, room #, and location of drain you're removing! While Unsterile Sterile +/- post-pull CTH as warranted (per chief) - TELL NURSE AND PLACE ORDER |
How to remove Bolts
| MATERIALS | PROCEDURE |
Materials:
| Do a mini time-out with yourself. Confirm the patient, room #, and location of drain you're removing! While Unsterile Sterile +/- post-pull CTH as warranted (per chief) - TELL NURSE AND PLACE ORDER |
How to remove Lumbar Drains
| MATERIALS | PROCEDURE |
Materials:
| While Unsterile 1. Remove tegaderms and all pressure dressings over drain 2. Chloroprep the area where drain is coming out Sterile (wear your gloves) 3. cut out all securing sutures 4. SLOWLY pull out the drain. It should pull out very easily. Do NOT GO FAST, that is how you shear the tubing against some bony structure or something. 5. Tie down buddy stitch or throw in a figure of 8 or purse-string around site. |
How to remove spine drains
Spine drains will be HMV most often.
| MATERIALS | PROCEDURE |
Materials:
If Gerszten: nylon suture + Kelly | None of this has to be sterile*
*Gerszten want buddy stitches around drains, follow sterile procedure as above for cranial drains, throw in a simple interrupted (just one poke, doesn't have to be a figure of 8), then dress with primapore). |
How to change EVD or LD Buretrol
You will often have to do this when the tubing cracks.
| MATERIALS | PROCEDURE |
Blue towels x 2 (2-3 more if you are priming the buretrol Sterile gloves Silk tie Hemostat Suture removal kit Small chloroprep sticks x 2 Buretrol (Exacta drainage system) | 0. Prime the buretrol (if in ICU, nurses will do this for you) and place it on sterile blue towel side table Pre-sterile 1. Drop materials onto sterile blue towel field 2. Place blue under connection between EVD (red tubing) and buretrol (clear tubing) where there is a silk tie. Sterile 3. Contaminate your left (or non-dominant hand) to lift up dirty connection off of blue towel 4. Use sterile hand to wipe down the orange-white connection 5. Clamp EVD (orange tubing) with hemostat 6. Use scissors to cut silk tie 7. Unscrew EVD nipple from buretrol (clear) tubing 8. Use new chloro-prep stick to wipe the open (but clamped) EVD nipple connection 9. Bring new buretrol onto patient while keeping the cap on clear tubing until you remove with your sterile hand 10. Connect sterillay the EVD nipple to new tubing 11. You are done being sterile 12. Reinforce with a silk tie |
Often you will send CSF too once the tubing is cracked to ensure no infection, but ask your chief.
How to remove central lines / PICC
Firstly, you can always place a consult to the IV Team to do this for you, the order is "IV Team Consult" and you just choose what you want them to take out. Generally you should try this at the beginning of the day if there is time for the IV team to do it.

In case IV Access Team does not make it or it's the weekend or you just want to get it out of the way yourself, here is how to do it.
Materials:
Xeroform dressing, 4 x 4s, suture removal kit, chloroprep, sterile gloves. Have a nylon suture and hemostat but don't open, use stitch PRN if the incision was too big and keeps oozing.
1. Position patient in Trendelenburg (head DOWN). DO NOT DO THIS WITH THE PATIENT SITTING UP, THEY CAN ACTUALLY DIE FROM AN AIR EMBOLISM THIS IS NOT A MYTH.
2. Remove dressing unsterilley.
3. Chloroprep the area w/ small chloroprep stick and put on sterile gloves.
4. Cut sutures
5. Once you start literally pulling it out, tell the patient to hum and hold their hum it while you are taking it out .
6. Occlusive xeroform dressing --> gauze --> Tape down (tegarderm)
7. Patient can stop humming once out and occlusive dressing is over.
8. Ideally hold pressure for 5 minutes (not extremely necessary if too busy).
9. Tell patient to lay flat for 20 minutes.
There should be NO resistance. If there is, STOP, place occlusive dressing, and call for help.
How patient will present if they get an air embolism: instant death vs. stroke. If stroke symptoms, call condition C and tell them you are worried about air embolism, how do we get hyperbaric ASAP (hint: next to escalators in lobby).
How to reprogram shunts
Medtronic - Analog Dialer
Medtronic - Electronic
Codman
What to do after a needlestick incident
TBA
How to sign out to night floater
| Scenario | Instructions |
| General Template |
NOTE: BEFORE you sign this out make sure everything is appropriately ordered for the night-floater! And nurses are called, etc.You are to dump as minimal work as possible on the busy night floater. Example: Jo Johnson in 4G bed 5, check 4am scan which is ordered. If epidural is enlarged, call attg / chief. |
| Post-op check / post-op imaging | If you do a case late, you can generally sign out the delayed exam and post-op scan to night-floater. Use this sparingly obviously and only if you are leaving the hospital. How to sign-out delayed post-op exam to night-floater - is the patient extubated? - does the attending / chief need to be woken up about the exam overnight? NOTE: this is obviously only a delayed exam you sign-out. you still examine immediately after and get the most useful exam that you can even if patient still waking up, it's useful to know they are MAEx4 and pupils are reactive. - What to look for on scan (usually obvious, bleeding, etc.) |
| Sodium management (for both HYPER and HYPO-natremia) | This will be common on blue services but also may happen on every service. 1. Triple check that sodiums are ordered at the interval you want overnight and know at exact times night-floater can expect to happen (e.g. q4H sodium next is 10PM then 2AM). Then call overnight nurse (they hand-off at 7) and ensure she is aware sodium is ordered for these times). Can kindly ask her to text-page the night-floater if you want. 2. What is most recent sodium before you are signing out 3. What is the sodium goal (e.g. normonatremia, Na+ > 145) 4. Know who is managing (Endo vs. Renal vs. NSGY), i.e. does the nigh-floater call renal vs. just make the change themselves? 5. Have an algorithm for what action to take. e.g. turn off fluids if Na+ drops below 135, etc. |
How to handle weekends at Presby
How to document / report CSF Studies
Do this anytime CSF is obtained from LP/EVD/Shunt tap
P1 procedure (OP = , RBC/WBC/glucose/protein/gram stain / Cx)
How to interpret a UA
TBA
How to check if a trach is cuffed / cuffless
TBA
General Survival Tips
- Running through plans in AM with charge nurse on every floor is extraordinarily high yield. They will like you and also help you get shit done, they know who to call for random shit better than you do and want to advance patient care and discharge people just as much as you do.
Principles of surgical positioning
How to pin and unpin patient heads
TBA
How to flip a patient
Align breast pads on sternum etc. TBA
Cervical spine
Thoracic spine
Lumbar spine
How to un-flip a patient
If head is pinned: keep arms tucked and patient taped until
How to position and tuck arms
Above T4: arms down
- Thumbs always must be pointing down (TBA picture).
T4 and below: superman (TBA picture)
How to manage tube during flips
TBA
Closing an incision: A Layer by Layer Guide
General tips:
- Always start AWAY from yourself if possible
- Do corners and then middle first
- If long incision, use markers
- If incision is small or difficult to see, can consider not tying until the end and just snapping your stitches
Buried knots
| Bite 1: DEEP to SUPERFICIAL (on your side) | Bite 2: SUPERFICIAL to DEEP (on opposite side) |
 |  |
- When tying: sinch "sideways" on the second tie
Non-buried knots
- Everything is opposite from buried
- bite 1 on opposite side: superficial to deep
- bite 2 on your side: deep to superficial
- when tying: sinch "up" with your post
General tips on closing skin anywhere
DOG EARRING
- definition: when you advance UNEQUALLY along each side with your bites, you end up with extra incision on one side at the end
- How to prevent: advance equally
- How to correct:
- bit closer to edge of incision on site dog-earring, bite farther away from incision on side that is not dog-earring (TBA)
- may have to cut out some stitches to release some tension (TBA)
APPROXIMATING VERTICALLY MISALIGNED SKIN
- bite deeper in the lower side (BITE LOW on the LOW side)
- bite superficially in the higher side (BITE HIGH on the HIGH side)
STAPLES
- use Addy's to bring each side together vertically before every staple
- Staples 5-7.5 mm apart
GENERAL PRINCIPLES OF KNOTS
- Always tie your first two knots in same direction, then alternate every knot therafter
Q: HOW MANY KNOTS SHOULD I TIE?
A:
monofilament = ≥ 6 ties (easier to spontaneously unwind so need more)
poly-filament (braided) = 4 ties
Common sutures we use and their filament structure
| Suture | Type |
| Maxon | monofilament |
| Vicryl | polyfilament |
| Monocryl | monofilament |
| Nylons | monofilament |
Q: WHAT LENGTH OF TAIL?
A:
In the body (i.e. under skin), you want the minimum amount of foreign material so shorter is always better. But you also don't want to cut so close that you compromise the knot and make it start unwinding.
On skin (outside the body), just keep a long tail (~1cm), it doesn't hurt.
SPINE: LAYER BY LAYER
| LAYER | BURIED KNOT? | Suture to ask for | Technique | Ideal pickup | Comments / Tips |
| Muscle | NO | NON-absorbable (prolenes) or Absorbable (Maxon) | Simple interrupted +/- superimposed running +/ - figure of 8 +/- V-lock (braided locking stitch)
| Rat tooth gerald | Often close muscle in same bite as fascia; technically closing muscle not strictly necessary. |
| Fascia | NO | Rat tooth gerald |
| ||
| +/- Fat or Scarpa | + / - depends on distance from skin | Rat tooth gerald or Addison w/ teeth | technically "useless" for closure but in really fat people, can close dead space where a seroma/infection may otherwise form | ||
| Deep dermal | YES | 3-0 or 2-0 vicryl (polysorb) or maxon/prolene also sometimes used | Simple interrupted | Addison |
|
| Skin | N/A
| Absorbable (monocryl or biosyn) Non-absorbable (nylon)
| Absorbable
Non-absorbable (nylon)
Other Subcuticular V-lock or stratafix | Addison |
|
CRANIAL: LAYER BY LAYER
| LAYER | KNOT | Suture to ask for | Technique | Ideal pickup | Comments / Tips |
| Bone | pterional crani - anterior/superior occipital: superio-medial | ||||
| Dura | |||||
| Galea | |||||
| Skin |
CHEST (batteries): LAYER BY LAYER
| LAYER | KNOT | # Ties in KNOT | Tail Length | Suture to ask for | Technique | Ideal pickup | Comments / Tips |
| +/- Fat | |||||||
| Deep dermal | |||||||
| Skin |
Abdomen / Thigh
TBA
Drain stitches
TBA
How to transfer patient to Medicine
Rules:
- TBA
Tips:
- TBA
How to handle common nursing pages
Always physically see the patient before you talk to your senior about them.
| Pager Chief Complaint | What to ask nurse on phone before seeing pt. | What to ask patient. | What to examine. | Management BEFORE call chief* |
| Neuro exam change | turn off sedation and paralysis now and please have a train of four and pupillometer ready. | everything | NOTE: this is exception to rule of ordering things before talking to senior. Talk to a senior before ordering a CTH unless it is a profoundly obvious exam change. | |
| Not protecting airway | Call respiratory ASAP for suctioning and go see immediately. | Condition and ICU transfer | ||
| "I think they just aspirated" | Ok I will order a stat CXR | CXR
| ||
| Intractable vomiting | When was the last time? How many times? was it after eating? Did they aspirate the vomitus or clear it? | Add more anti-emetics (see HY pharm chart) Make sure not aspirating | ||
| HYPO-tension | Did you repeat check on other arm? Is BP cuff size appropriate? What meds on? | Symptomatic? HA, drowsy, etc. |
| |
| HYPER-tension | Do they take any home anti-HTN? Were they in pain when you measured? Did you give labetalol / hydralazine | Is your pain well-controlled? Red flag signs for hypertensive emergency AMS Headache Blurry vision Vision loss Chest pain Palpitations Sweating SOB Nausea / vomiting Back pain? | Restart home anti-HTN + / - medicine consult Condition and ICU if legit HTN urgency / emergency End-organ damage orders CT scan if ischemic / hemorrhage stroke concern EKG / Echo for MI / HF CXR for pulm edema Renal consult if hematuria U/S or CTAP if have known aortic aneurysm Optho consult for DFE if vision changes | |
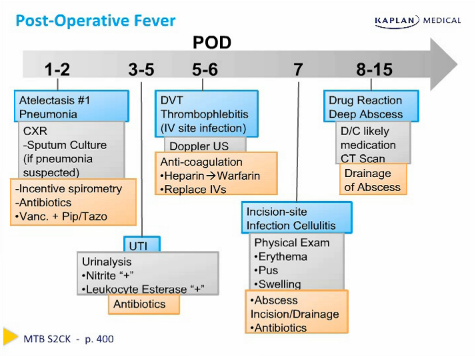
Febrile (see chart for post-op fever timeline below) | can you recheck a core temp (rectal) What is the actual temperature? A true fever is 38.5 / 101.3 | basic fever workup: ESR, CRP, CXR, UA, BCx if you want them and LEDs | ||
| Hyperglycemia | Endo consult for insulin mgmt Remember ADA guidelines for hospitalized patients are 140-180. | |||
| Hypoglycemia | Endo consult for insulin mgmt Make sure all home PO meds are held | |||
| Chest pain | Are they anxious? Are they having pain? | Crushing? | Is it reproducible? | EKG, trop, lytes CXR |
| Diarrhea | Is it truly watery? How many times in past 24 hours. Does it smell like C diff? | C diff test if 3 liquid BM in < 24 hrs | ||
| Leg pain / swelling | Ask about all vitals (tachycardia, tachypnea) uncomfortable breathing? | swelling erythema sweaing | painful? SOB? Chest pain?
| CTPE if c/f PE LED
|
| Arm swelling | Was there an IV there? Is it infiltrated? Is it painful? | swelling erythema | Monitor + / - UED | |
| Abdominal pain | distended? Hard? rebound tenderness? | Abdominal Xray if ALIF patient, very low threshold for ACS consult or STAT page to general surgery team that operated with us. | ||
| Uncontrolled pain in spine |
| oxy5 for mild pain oxy10 for moderate pain dilaudid for breakthrough pain norco or oral hydromorphone is alternative to oxy (shortage) AIPSS consult | ||
| Uncontrolled pain in cranial | ||||
| Urinary Retention | Straight cath if PVR > 400 cc UA | |||
| Family wants to talk to a doctor | If you are extraordinarily busy (not just being lazy) and it is just a gomey question not related to patient being sick, you can kindly ask nurse to put the family on phone. | |||
| Patient is leaving AMA | ||||
Recall timeline for post-operative fever (blue), with diagnostics (gray) and management (orange).
Death Summaries and Death Paperwork
0. Notify rapid response 864-2860
1. Get a red packet from charge nurse on floor in which patient died and fill out boxes 23a-39c. The attending/fellow who announces death will need to sign box 23.
2. Call Alllegheny Medical Examiner 412-350-4800. Call with the chart open as they will ask for circumstances of death and clinical info. You will also need to have the following info on hand:
- Patient home address and home phone number (Patient Information on Powerchart)
- Next of kin and phone number (Caredex)
3. Return red packet to charge nurse on floor.
Make sure all of this is meticulously filled out. If not, you will get calls about this weeks later asking about the patient you have forgotten about.
Rules for conscious sedation at Presby
Intubated patients: can receive multiple doses or classes from their sedative drips.
Non-intubated patients:
From Hafeez (NICU Medical Director): Patients in whom you are performing a bedside procedure: EVD, lumbar drain, lumbar puncture etc OR giving medications prior to cerebral imaging, the use of 2 sedatives in different classes OR the use of 1 sedative and 1 analgesic medication at the time of the procedure or imaging constitutes conscious sedation.
Conscious sedation requires the presence of the CCM team* OR the Neurosurgical attending.
Conscious sedation is a specialized form of anesthesia that carries specific criteria for airway and hemodynamic monitoring and hospital privileges. Please be careful of what medications you order for beside procedures or imaging.
*Has to be CCM faculty. The fellows and residents can help or be there but CCM attendings have to be present.
Ordering Pitt NSGY Jackets
This is the responsibility of your intern class. Specifically, the block 1 pathology/ICU intern needs to spearhead this ASAP and have jackets delivered by end of block 1 or early block 2 at the latest (handing off the work to Block 2 path/ICU intern).
1. Discuss among your intern class what jacket candidates you like, and order 4-5 jackets for chiefs to see physically. Options for payment: ask one of the chiefs for their credit card, ask Missy for the UPMC card, or buy it yourself. Features that are highly desirable:
- breathable (should be an indoor midlayer)
- sleeves roll up easily (so easy to examine patients / do things with your hand and wash above your wrist.
- small external pocket for airpods
- internal pockets for things like a scrub cap
- sleek and mobile
- big enough company where it will be easy to get 20-30 jackets (don't buy some super niche brand)
- Aim for $150 max, $200 is pushing it and better be worth it.
Historical brands: (choose something different or people will complain)
2023-24: Helly Hansen
2022-23: lululemon
2021-22: Arcteryx
2. Chiefs will choose from your selection. (In general it is better to order widely so that chiefs cannot turn them all down and make you order more, delaying everything).
3. Once you have a final chief choice, order men's samples S/M/L/XL and usually female samples XS/S/M is enough, and give them to Missy.
4. Missy will email everyone to come try on and place an order in her office - generally this will be 2 weeks try-on period.
5. The path/ICU intern will be responsible for ordering ONLY RESIDENT jackets. Some attendings and other staff (APPs, admin) may ask but that is all up to Missy.
6. How residents place an order: the path/ICU intern is responsible for ordering and collecting all resident payments. First decide whose card you will use, it will have to be either a chief or your personal credit card. It should be easy to use your own credit card as residents must pay instantly for their order to be placed. Once you have decided whose card you will use, come up with a payment scheme (e.g. people pay you on Venmo and then you place their order with your card).
7. Intern places all orders for residents, consolidates jackets from Missy, and send an email to all who ordered confirming their size and what will be embroidered. Give everyone 1 week to respond to this email, by default everyone will get their last name and can reply to you if they want no name embroidered or something else. Here's the template for how to email this:
| Resident | Size / Gender | Embroidered text |
| Resident 1 | Small / Female | Last Name 1 |
| Resident 2 | Medium / Male | Last Name 2 |
8. Intern label every tag with the embroidered text, imperative that you are careful with spelling and that appropriate sizes are labeled with the correct person's name!
9. Intern takes all orders to Monogram It 412-967-9500 1310 Freeport Road Pittsburgh PA 15238
10. Monogram it will take 2-3 weeks and then bill Missy, who will then charge everyone (it's about $17 per jacket for name and Pitt Logo).
11. Intern picks up embroidered jackets and brings to Missy's office.
How to order equipment from IT
Orientation to-dos before starting intern year
- Schedule opioid training with Missy ASAP so you can prescribe opioids
- Setup PT/OT forwarding
- Setup Case manager email forwarding
- Download contact list and change pagers to your own phone number
- Cell phone apps
- Avaya Workplace App
- SPOK Mobile on phone
- Doximity app
- MDoc+
- Microsoft 365
- To Do App
- UpToDate
- VIP Access app
- Cerner To-dos
- Setup note type filters:
- Service specfic: ENT, optho, Endo, PMR
- Type:
- procedures
- OP note
- Setup templates:
- Progress notes
- Discharge Summaries
- EVD Note
- LD Note
- LP Note
- Shunt tap note
- Shuntogram note
- Setup note type filters:
Favorite Orders
1. Click on Provider Home/Quick Orders
2. Click on tab that says Hospitalist Quick Orders on the top
3. In the right search bar that says “Provider Last name, First name” enter the resident that you will copy order sets from.
4. Select into the folder and click “Order” for each one to copy.
5. Go into “Orders” in the left navigation panel.
6. Click “Orders for Signature” in the bottom right corner.
7. Highlight all orders. (Shift + select)
8. Click Add to Favorites
9. Click on “New Folder”, rename it into a folder, then press “Okay”
10. Press the refresh button at the top right corner and say “Yes” to cancel the orders.
NSGY Textbook OneDrive library
To Do List Template (TBA)
Cheat Sheet printout (TBA)
Consult Template (TBA)
- Setting Up A Surgery ("PCS")
- Sign-off template
- Plan A - Cranial
- Plan A - Spine
- Workflow for discharging a patient
- High yield pharmacology guide
- How to drug people for an LP
- How to drug people for an MRI
- How to intubate people for an MRI
- Steps BEFORE Every Case
- Steps AFTER Every Case
- How to preround
- How to present
- Neuro exam template
- Post-Angio Check
- How to setup patient for angio
- How to coordinate shunt with general surgery
- How to schedule IR-guided LP or CT-Myelogram at PUH
- How to schedule inpatient EMG/NCS at PUH
- How to stand a patient for an Xray
- How to call a condition C (critical) at Presby (Orange bag)
- How to call a stroke condition at Presby
- How to place a duo-tube
- How to order tube feeds
- How to handle Answering Service like a champ
- How to place a duo-tube
- How to remove cranial drains
- How to remove EVDs
- How to remove Bolts
- How to remove Lumbar Drains
- How to remove spine drains
- How to change EVD or LD Buretrol
- How to remove central lines / PICC
- How to reprogram shunts
- What to do after a needlestick incident
- How to sign out to night floater
- How to handle weekends at Presby
- How to document / report CSF Studies
- How to interpret a UA
- How to check if a trach is cuffed / cuffless
- General Survival Tips
- Principles of surgical positioning
- Closing an incision: A Layer by Layer Guide
- How to transfer patient to Medicine
- How to handle common nursing pages
- Death Summaries and Death Paperwork
- Rules for conscious sedation at Presby
- Ordering Pitt NSGY Jackets
- How to order equipment from IT
- Orientation to-dos before starting intern year


