Moossy Carpal Tunnel Release
Anatomy
The incision is linear, between the thenar and hypothenar eminences at about the level of the space between the 3rd and 4th fingers. The proximal end is at the wrist crease and it extends 4 cm distally.

The recurrent branch of the median nerve innervates the thenar eminence. It branches off the lateral median nerve distal to the carpal tunnel.

The transverse carpal ligament inserts on four carpals: on the ulnar side it inserts on the hamate distally and the pisiform proximally and on the radial side on the trapezium distally and the scaphoid proximally.
In addition to the median nerve, the carpal tunnel contains the eight tendons of the flexor digitorum profundus (4) and flexor digitorum superficialis (4) as well as the single tendon of flexor pollicis longus.

Positioning
Supine on a regular table, relevant arm extended at a 90-degree angle. Bed is turned such that the arm is away from anesthesia.
Prep
Prep before the patient goes to sleep. Ask the patient to raise their arm, then prep from the fingertips to the shoulder.
Draping
- Unroll a stockinette over the hand and down the forearm and arm
- Place a drape on the armboard followed by a blue towel nearest the patient's axilla
- Ask the patient to let the arm rest on the arm board
- Place another blue towel on top the shoulder
- Secure the top blue towel to the one under the arm with towel clips above and below
- Pass the arm through the arm-hole of the carpal tunnel drape and pass the "up" part to anesthesia




Medications
Cut through the stockinette with scissors to expose the arm. Infiltrate the planned incision with lidocaine. Moossy does not like epi.
Procedure
The procedure is done sitting on a stool. Moossy prefers if you sit on the radial side (i.e. the side of the thumb).
Be sure to supinate the hand.
Make the skin incision with a 15 blade, going through the skin to the subcutaneous tissue.
Place a self-retaining retractor.
You will next encounter the palmar fascia, the insertion of the palmaris longus tendon. The fibers of the palmaris fascia are radially oriented from an origin point at the base of the palm. Continue to incise this with the 15 blade, along the same line as the skin incision.
Next, the transversely-oriented fibers of the transverse carpal ligament are encountered. Continue incision with the 15 blade until you are through it and can see the median nerve in the carpal tunnel.
Re-orient your body such that you are seated at the end of the arm board, furthest from the patient, with your line of sight going down the arm. Use the non-toothed end (i.e. not the rake) of a Sen retractor to retract the skin and soft tissue of the proximal corner of the incision (i.e. nearest the wrist). Pull up on the Sen retractor towards the ceiling. This both widens your view and causes the median nerve to pull deep, away from the flexor retinaculum.
Use Metzenbaum scissors. With the tips closed, dissect the space between the flexor retinaculum and median nerve. Do not spread. With small snips, open the flexor retinaculum towards the wrist. Pass a 4 Penfield into the carpal tunnel and attempt to pass it under the skin into the forearm. The proximal ligament is completely release when the tip of the 4 Penfield passes easily into the subcutaneous tissue of the forearm.
Reorient your body such that you are seated alongside the patient, in the axilla. Again use the blunt end of the Sen retractor to retract the skin and soft tissue directly upwards, towards the ceiling. Using the same technique, dissect the space between the flexor retinaculum and median nerve with the closed tips of the Metzenbaum scissors then carefully cut through the ligament. the distal decompression is complete when you see fat.
Closure
Do not close the flexor retinaculum. Use a single layer of 3-0 Nylon interrupted suture to close the skin and soft tissue.
Dressing:
- Bacitracin ointment
- Xeroform over the incision
- "Fluffed" 4x4 gauze
- Webril wrap
- Ace bandage
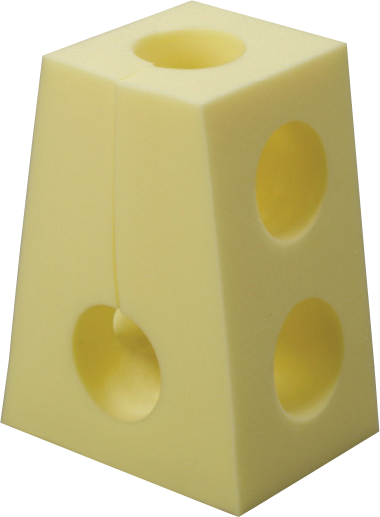
- "Swiss cheese" yellow foam arm support
Postop
Patients go home the same day. The bandage stays on for 3 days then can be removed and the patient can shower. Send home with two 5 mg tablets of oxycodone. Most pain can be controlled with Tylenol. Return to clinic in 2 weeks for a wound check.
